The following case documentation shows the pre- and postoperative course of the treatment of a patella fracture. In the 35-year-old patient, an unfortunate step causes a transverse fracture of the distal patellar pole. After a walking cast and relief for 4 weeks, a refracture occurs at the identical site, and a cast is applied again for 8 weeks. A pseudarthrosis appears, which is to be treated surgically with a Shark-Screw® graft 5.0. 6 months postoperatively, the pseudarthrosis shows very good healing. The patient is symptom-free.

X-ray image preoperatively
The control X-ray clearly shows the pseudarthrosis

X-ray postoperatively
Treatment of the patella fracture with a Shark Screw® Graft 5.0mm
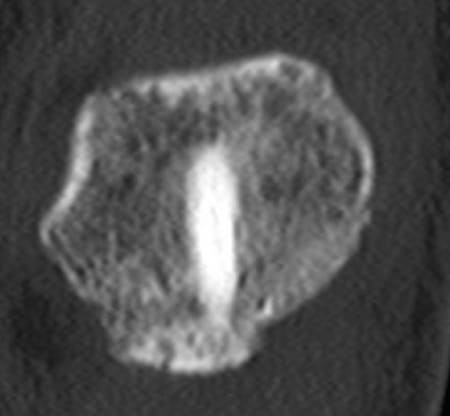
CT 4 months postoperatively
The Shark Screw® is firmly healed and still visible.

CT 4 months postoperatively
The Shark Screw® has already been partially incorporated into the patient's own bone
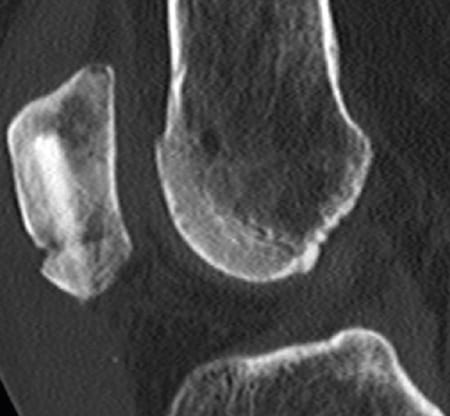
CT 4 months post-operatively
Pseudarthrosis healed very well
Other supply methods
Currently, the treatment of patellar fracture with the K-wire is widely used. Many authors cite a cerclage with K-wire as the most common method. Delayed wound healing or wound healing disorders, knee stiffness, prolonged inability to work and severe limitation of movement are associated with this method of treatment. Other symptoms and complications described range from K-wire fractures, soft tissue irritation and injury, and K-wire migration to erupted patellar fragments. Some authors recommend a combination of screws and KWire. In addition, authors report complication rates ranging from 5% to 32.5% for the K-wire or K-wire-and-screw method. In view of the high complication rate, the relief of patients by new methods would be desirable.
Case documentation
The following case involves a 35-year-old female patient. She is active in sports. The initial contact was made on July 18, 2017. The patient had recent overload from dancing for several hours. The MRI confirmed the suspected diagnosis of bone bruise; however, a few hours after the MRI, an unfortunate step caused a transverse fracture of the distal patellar pole. After a walking cast and relief for 4 weeks, a refracture occurs at the identical site, and a cast is applied again for 8 weeks. The control X-ray (Fig. 1) clearly shows the pseudarthrosis, which is to be surgically treated with a Shark-Screw® Graft 5.0. After median skin incision with exposure of the fracture gap from the dorsal side and sparing of the extensor apparatus, a relatively tight pseudarthrosis is seen. The fragments are freshened with a sharp spoon and several tapping holes on either side of the planned screw position. The patella parts are fixed and compressed with reduction forceps, then a guide wire for the Shark Screw® is inserted centrally from distal to proximal under BW control. It is drilled out to 5mm with increasing sizes and the thread is cut by hand with the Shark-Screw® instruments. The canal is carefully flushed, then a 5mm Shark Screw® is inserted under BW control. The protruding screw head is removed by means of the oscillating saw. Any residual supernatant usually resorbs within the first 6 months. A layered wound closure without drainage and a postoperative final X-ray were performed (Fig. 2). The patient’s follow-up treatment was extremely conservative with TENS unit, SecuTec® splint for 10 weeks, release of flexion in 10° increments from the 3rd week, active physiotherapy from the 6th week and partial weight bearing for 6 weeks with 20kg. 6 months postoperatively, the pseudarthrosis has healed very well, the remodeling of the Shark Screw® into the patient’s own bone has already been partially completed, the rest of the Shark Screw® is firmly healed and still visible (Figs. 3 to 5). The patient is symptom-free.

